Health
India is now being rated as a Better Place for Chemotherapy Treatment

Cancer is a deadly disease and it has become so common these days, that every 1 in 10 people suffer from it. In earlier days, treating cancer was very tough as there were not much inventions in the cancer treatment. With the advancements made in the field of cancer in this era, it is possible to fight cancer and win over it.
One of the treatment that is widely used in treating cancer is chemotherapy and one of the affordable destination for the treatment is India.
To know more about the cost of chemotherapy in India, Click Here. Clinicspots is an online medical Question/ Answer platform and a medical facilitator that makes medical knowledge more accessible to the masses. You will get all your queries cleared on this platform regarding chemotherapy.
Chemotherapy helps to stop or slow down the growth of the cancer cells. What makes it as a widely used treatment is that it not only kills the cancer cells in a particular part of the body but, also works for the entire body. It kills the cancer cells that are existing in the whole body.
Well, what can make your nights sleepless, is the cost of chemotherapy. The cost of chemotherapy is huge making it difficult to pay for the treatment. In countries like US, one chemotherapy cycle can cost you around $10,000.
Basically, the cost of chemotherapy around the world is very high and usually out of reach for its own citizens. However, there are places where you can get affordable chemotherapy like India.
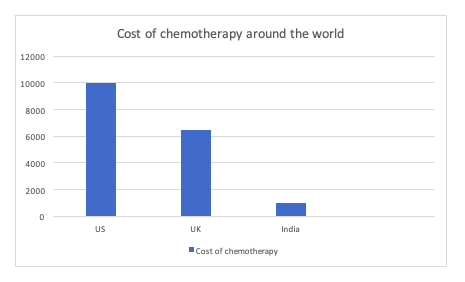
While comparing the cost of chemotherapy of multiple countries, you will find out that India provides the most affordable treatment. What makes the cost of treatment so low in India, is the currency.
The currency of India is low as compared to the other currencies like dollar and euro. This makes the cost of living in India very low and hence, the cost of treatment is low.
Apart from this, there are other factors that influence the cost of chemotherapy in India.
Like, you can be given chemotherapy orally, IV (intravenous) or through port. How you will be delivered chemotherapy depends on your type of cancer and stage.
Oral chemotherapy is the most economical treatment as it does not involve any equipment while chemotherapy given through port is the most expensive as it involves a minor surgery and equipment.
Now, let’s discuss what makes India, an ultimate medical destination for getting chemotherapy
- High quality treatment

The treatment that is offered in India is of very high quality. The doctors here are extremely knowledgeable and experienced in their field of specialisation. They have graduated from the best medical institutes in the world.
In addition to this, are the hospitals. You will get a large number of hospitals to choose from. All the cancer hospitals in India offer high quality treatment.
- Latest technology

Well, while getting treatment, we always search for hospitals that have latest technology. India, like any other developed country has all the latest technology based equipment. Some examples of ultra – modern medical equipment are proton therapy, cyberknife, gammaknife, etc.
- Treatment at a very affordable cost
We have already discussed the cost of chemotherapy in India. As we have seen, the cost in India is comparatively very low as compared to the other countries.
Even if you add up all the expenses which includes treatment, travelling, food and stay expenses, your total expenses will be very less as compared to the other developed countries.
- World class services
The services offered in India are of international standards. You even get a translator so that you are more comfortable in communicating. The services provided here, can be customised as per your choices.
These factors make India one of the most visited place for chemotherapy.
Health
BioLongevity Labs: How Two Biohackers Are Making Longevity Safe for the Mainstream

Humans have been looking for ways to extend their lifespan for hundreds of years. Medicine has made impressive strides, but for many, the effects of aging are still painfully real.
Through BioLongevity Labs, biohackers and entrepreneurs Jay Campbell and Josh Felber aim to introduce ordinary people to potentially life-changing compounds called peptides. Campbell and Felber come from very different backgrounds.
Campbell is a five-time international bestselling author and globally recognized leader in the health-optimization space. Felber is a serial entrepreneur who excels at scaling businesses.
For both men, BioLongevity Labs is more than just a business venture — it’s about helping everyday people discover something that just might prolong and improve their lives.
“Your body inevitably changes as the years pile on,” says Campbell. “Your energy drops, and wrinkles start showing up uninvited. Peptides can change everything.”
Many people have probably heard the term “peptide” in passing. Some may know they’re associated with longevity. Most people just don’t have a strong grasp of how they work.
A peptide is a short chain of amino acids, which are the building blocks of proteins. Essentially, peptides are like shorter, simpler proteins. That might sound unremarkable, but the real magic of peptides lies in how they work.
They function as signaling or “messenger” molecules telling the body to perform specific functions. Many peptides function similarly to hormones. A relevant example is GLP-1 (glucagon-like peptide-1) receptor agonists. This class of medications includes semaglutide and tirzepatide, two wildly popular weight-loss drugs.
“These peptides aren’t just another biohacking fad,” Campbell explains. “They enhance insulin secretion and suppress glucagon release to balance blood sugar levels and promote sustainable weight loss”. But what sets GLP-1 receptor agonists apart is their ability to regulate hunger.
Through the reduction of appetite and increased feelings of fullness, it is far easier for dieters to stick to a calorie deficit.” Although GLP-1 receptor agonists are widely prescribed, most peptides aren’t.
Campbell asserts, because many peptides have the potential to cure illnesses by treating the fundamental root cause, they go against America’s “sick care” model of healthcare. They potentially threaten drug companies and their bottom line.
“Peptides are simultaneously a dream come true for mankind and the worst possible nightmare for the pharmaceutical industry,” says Campbell. “It’s not a conspiracy theory. It’s pure economics and psychology in action. People will do whatever it takes to make as much money as possible in a free-market society, even if it means suppressing a superior solution.”
Patients probably aren’t going to be introduced to peptides through the healthcare system. Many discover them on their own. But for the many people who don’t have a solid understanding of how they work molecularly or even what dose to take, there is a risk. That’s precisely what BioLongevity Labs’ co-founders are attempting to address.
Jay Campbell has dedicated his life to educating people about therapeutic peptides and optimized hormones, and along with his partner Josh Felber, they’ve created a company offering filler-free, third-party tested peptides and bioregulators.
Campbell and Felber stress the fact that BioLongevity Labs isn’t meant to be a replacement for traditional medical care. Instead, its products bridge the gap between clinical and extra-clinical care. There’s no magic pill or single solution to solve the problem of aging.
But thanks to the development of specialized peptides, bioregulators, and small molecules, we’re closer than we’ve ever been before.
-

 Tech5 years ago
Tech5 years agoEffuel Reviews (2021) – Effuel ECO OBD2 Saves Fuel, and Reduce Gas Cost? Effuel Customer Reviews
-

 Tech6 years ago
Tech6 years agoBosch Power Tools India Launches ‘Cordless Matlab Bosch’ Campaign to Demonstrate the Power of Cordless
-

 Lifestyle7 years ago
Lifestyle7 years agoCatholic Cases App brings Church’s Moral Teachings to Androids and iPhones
-

 Lifestyle5 years ago
Lifestyle5 years agoEast Side Hype x Billionaire Boys Club. Hottest New Streetwear Releases in Utah.
-

 Tech7 years ago
Tech7 years agoCloud Buyers & Investors to Profit in the Future
-

 Lifestyle5 years ago
Lifestyle5 years agoThe Midas of Cosmetic Dermatology: Dr. Simon Ourian
-

 Health7 years ago
Health7 years agoCBDistillery Review: Is it a scam?
-

 Entertainment7 years ago
Entertainment7 years agoAvengers Endgame now Available on 123Movies for Download & Streaming for Free
